Recent quotes:
Mindfulness meditation reduces pain by separating it from the self: UC San Diego study reveals neural circuitry supporting mindfulness-induced pain relief -- ScienceDaily
The study, published July 7, 2022 in PAIN, showed that mindfulness meditation interrupted the communication between brain areas involved in pain sensation and those that produce the sense of self. In the proposed mechanism, pain signals still move from the body to the brain, but the individual does not feel as much ownership over those pain sensations, so their pain and suffering are reduced. "One of the central tenets of mindfulness is the principle that you are not your experiences," said senior author Fadel Zeidan, PhD, associate professor of anesthesiology at UC San Diego School of Medicine. "You train yourself to experience thoughts and sensations without attaching your ego or sense of self to them, and we're now finally seeing how this plays out in the brain during the experience of acute pain."Mindful breathing for pain control: Like Yin and Yang -- ScienceDaily
"(I was surprised) that both meditative breathing methods decreased pain sensitivity, but oppositely in the brain, like yin and yang," DaSilva said. "One by engaging the brain in an immersive exterior 3D experience of our own breathing, or exteroception -- yang, and the other by focusing on our interior world, interoception -- yin."New study gives the most detailed look yet at the neuroscience of placebo effects -- ScienceDaily
"Our findings demonstrate that the participants who showed the most pain reduction with the placebo also showed the largest reductions in brain areas associated with pain construction," explains co-author Wager, who is also the principal investigator of the Cognitive and Affective Neuroscience Lab at Dartmouth. "We are still learning how the brain constructs pain experiences, but we know it's a mix of brain areas that process input from the body and those involved in motivation and decision-making. Placebo treatment reduced activity in areas involved in early pain signaling from the body, as well as motivational circuits not tied specifically to pain."Comparison of the effect of photobiomodulation therapy and Ibuprofen on postoperative pain after endodontic treatment: randomized, controlled, clinical study | SpringerLink
It may be concluded that the use of photobiomodulation therapy was effective in reducing pain within the first 24 h when compared with the administration of Ibuprofen 600 mg.Capsule Commentary on Odineal et al., Effect of Mobile Device-Assisted N-of-1 Trial Participation on Analgesic Prescribing for Chronic Pain: Randomized Controlled Trial | SpringerLink
In this study, Odineal and colleagues1 examined changes in prescription analgesic prescribing for approximately 200 patients with chronic pain randomized to either a mobile app–enabled N-of-1 study (tailored, individualized pain-control interventions) or a control group. The app allowed patients to choose two treatment plans to compare over several short trials, selecting from a list of commonly prescribed analgesics or non-pharmaceutical therapies such as yoga or physical therapy. Among intervention patients, the authors found a clinically and statistically significant decrease in NSAID prescriptions relative to controls. Nearly one-quarter of intervention patients stopped NSAIDs during the study period, and the between-group difference was also significant.Statins, pain, glutamate (relates to leg pain post caffeine?)
The McMaster research team found muscle cells treated with statins released the amino acid called glutamate at much higher levels than muscle cells that were untreated. As glutamate is a potent activator of muscle pain receptors, this release was proposed to trigger the sensation of muscle pain. Thomas Hawke, senior author of the study and a professor in pathology and molecular medicine at McMaster University said: "We found that statins were able to enter the muscle cells and cause oxidative stress. This resulted in the muscle trying to increase its production of antioxidants to combat this stress. The side-effect of this antioxidant production was the release of glutamate out of the muscle cells."Treatment for chronic neuropathic pain gets to the brain via a novel route, without surgery - ScienceBlog.com
“We previously showed that in neuropathic pain, the accumulation of TNF in the brain, specifically the hippocampus, causes the dysregulation of the normal analgesic response,” said Ignatowski. “We propose that enhanced levels of TNF in the brain inhibit the release of norepinephrine. Normally, norepinephrine would activate the descending inhibitory pain pathway that projects to the spinal cord, thereby alleviating pain. But when activation of this inhibitory pathway is lost, pain may transition to a chronic state.” The new method originated with the UB researchers’ discovery in 1999 of TNF, a novel therapeutic target, specifically in the brain. They previously demonstrated that peripheral nerve injury—injury to the nerves connecting the spinal cord to the rest of the body—boosts levels of this protein in the hippocampus, a part of the brain responsible for learning and memory, and which they have recently found to be involved in the experience of chronic pain.Multiple brain regions moderate and link depressive mood and pain -- ScienceDaily
"We were very surprised about the expansive roles of these regions," said Zeidan. "Brain regions involved in facilitating pain were also associated with lower pain and depression. Brain regions involved in regulating pain where also associated with increasing depression. Perhaps it's not surprising after seeing the results. Why shouldn't specific aspects of the brain perform multiple roles?"I feel you: Emotional mirror neurons found in the rat -- ScienceDaily
On the basis of this, researchers formulated two speculations: (a) the cingulate cortex contains mirror neurons, i.e. neurons that trigger our own feeling of pain and are reactivated when we see the pain of others, and (b) that this is the reason why we wince and feel pain while seeing the pain of others. This intuitively plausible theory of empathy however remained untested because it is not possible to record the activity of individual brain cells in humans. Moreover, it is not possible to modulate brain activity in the human cingulate cortex to determine whether this brain region is responsible for empathy. Rat shares emotions of others For the first time, researchers at the Netherlands Institute for Neuroscience were able to test the theory of empathy in rats. They had rats look at other rats receiving an unpleasant stimulus (mild shock), and measured what happened with the brain and behavior of the observing rat. When rats are scared, their natural reaction is to freeze to avoid being detected by predators. The researchers found that the rat also froze when it observed another rat exposed to an unpleasant situation. This finding suggests that the observing rat shared the emotion of the other rat. Corresponding recordings of the cingulate cortex, the very region thought to underpin empathy in humans, showed that the observing rats activated the very neurons in the cingulate cortex that also became active when the rat experienced pain himself in a separate experiment. Subsequently, the researchers suppressed the activity of cells in the cingulate cortex through the injection of a drug. They found that observing rats no longer froze without activity in this brain region.Pain can be a self-fulfilling prophecy: New brain imaging research shows that when we expect something to hurt it does, even if the stimulus isn't so painful -- ScienceDaily
Unbeknownst to the subjects, heat intensity was not actually related to the preceding cue. The study found that when subjects expected more heat, brain regions involved in threat and fear were more activated as they waited. Regions involved in the generation of pain were more active when they received the stimulus. Participants reported more pain with high-pain cues, regardless of how much heat they actually got. "This suggests that expectations had a rather deep effect, influencing how the brain processes pain," said Jepma. Surprisingly, their expectations also highly influenced their ability to learn from experience. Many subjects demonstrated high "confirmation bias" -- the tendency to learn from things that reinforce our beliefs and discount those that don't. For instance, if they expected high pain and got it, they might expect even more pain the next time. But if they expected high pain and didn't get it, nothing changed.Cannabis Pain Relief Without the High - Neuroscience News
Cannabis indica and sativa are the two main cannabis strains that produce the pharmacological principles known as tetrahydrocannabinol (THC) and cannabidiol (CBD). Dr. Gabriella Gobbi’s team demonstrated that CBD does not act on the CB1 cannabinoid receptors like THC but through the mechanism that binds specific receptors involved in anxiety (serotonin 5-HT1A) and pain (vanilloid TRPV1). Researchers were able to extrapolate the exact dosage of CBD displaying analgesic and antianxiety properties without the risk of addiction and euphoria classically produced by the THC. “We found in animal models of chronic pain that low doses of CBD administered for seven days alleviate both pain and anxiety, two symptoms often associated in neuropathic or chronic pain,” says first author of the study Danilo De Gregorio, a post-doctoral fellow at McGill University in Dr. Gobbi’s laboratory.Sugar pills relieve pain for chronic pain patients: Placebo benefits can be predicted by brain anatomy and psychological traits -- ScienceDaily
About 60 chronic back pain patients were randomized into two arms of the study. In one arm, subjects didn't know if they got the drug or the placebo. Researchers didn't study the people who got the real drug. The other study arm included people who came to the clinic but didn't get a placebo or drug. They were the control group. The individuals whose pain decreased as a result of the sugar pill had a similar brain anatomy and psychological traits. The right side of their emotional brain was larger than the left, and they had a larger cortical sensory area than people who were not responsive to the placebo. The chronic pain placebo responders also were emotionally self-aware, sensitive to painful situations and mindful of their environment. "Clinicians who are treating chronic pain patients should seriously consider that some will get as good a response to a sugar pill as any other drug," Apkarian said. "They should use it and see the outcome. This opens up a whole new field."Mental imagery manages pain independent of opioid system: Study supports clinical use of mental imagery techniques in conjunction with pain-relieving drugs -- ScienceDaily
Mentally reframing pain as a pleasant experience is an effective regulation strategy that acts independently of the opioid system, finds new human research published in JNeurosci. The study supports clinical use of mental imagery techniques, such as imagining a new context or consequence of a painful event, in conjunction with pain-relieving drugs. Chantal Berna, Siri Leknes and colleagues tested two approaches toward modulating pain perception. For a mental imagery task, healthy men and women were instructed to imagine individually calibrated heat pain applied to their forearm as a pleasant experience, for example by thinking about warming up by a fire after coming in from the cold. A relative relief task used visual cues to manipulate participants' expectations about the forthcoming heat pain. Although both tasks made the pain experience more pleasant, only the effects of the relative relief task were blocked by naloxone -- the life-saving drug used to treat opioid overdose. Mental imagery was unaffected by naloxone, indicating that this approach works through opioid-independent mechanisms.'Mindful people' feel less pain; MRI imaging pinpoints supporting brain activity -- ScienceDaily
Whole brain analyses revealed that higher dispositional mindfulness during painful heat was associated with greater deactivation of a brain region called the posterior cingulate cortex, a central neural node of the default mode network. Further, in those that reported higher pain, there was greater activation of this critically important brain region. The default mode network extends from the posterior cingulate cortex to the medial prefrontal cortex of the brain. These two brain regions continuously feed information back and forth. This network is associated with processing feelings of self and mind wandering, Zeidan said. "As soon as you start performing a task, the connection between these two brain regions in the default mode network disengages and the brain allocates information and processes to other neural areas," he said. "Default mode deactivates whenever you are performing any kind of task, such as reading or writing. Default mode network is reactivated whenever the individual stops performing a task and reverts to self-related thoughts, feelings and emotions. The results from our study showed that mindful individuals are seemingly less caught up in the experience of pain, which was associated with lower pain reports." The study provided novel neurobiological information that showed people with higher mindfulness ratings had less activation in the central nodes (posterior cingulate cortex) of the default network and experienced less pain. Those with lower mindfulness ratings had greater activation of this part of the brain and also felt more pain, Zeidan said.When muscles weaken with age -- ScienceDaily
Working with our colleagues from the University of Aachen, we first systematically surveyed the changes taking place in the peripheral nerves of people aged between 65 and 79," Rudolf Martini describes his team's approach. During this, the researchers encountered an increased number of macrophages in the samples. Macrophages are cells of our body's immune system that engulf, digest and dispose microbes, foreign substances, cellular debris, aging cells etc. They set inflammatory responses in motion, help heal wounds and cleanse the tissue. Unfortunately, however, they also cause damage in some diseases. To find out whether this also applies to age-related nerve degeneration, the scientists performed an experiment on mice. "For this purpose, we looked more closely at the nerves of 24-month-old mice which is an advanced age for mice," Rudolf Martini explains. It turned out that the age-related changes in the mice's peripheral nerves are very similar to those in humans. As in their human counterparts, the number of macrophages was increased in the mice. Also, the older animals had less strength than their younger siblings and their motor endplates, the synapses connecting nerves and muscle fibres, were also less intact.Why It Matters How You Think About Pain | Outside Online
But the most interesting data deals with the difference between “adaptive” and “maladaptive” pain coping strategies. Adaptive strategies are things like ignoring pain, deciding that you won’t let it bother you, or overriding it with the urge to keep going. Maladaptive strategies are things like catastrophizing (“I’m going to have to drop out!”), fear (“It’s going to keep getting worse!”), and despondence (“This is awful!”). Each athlete was assigned daily composite scores of zero to six for adaptive and maladaptive coping, with zero corresponding to “never” and six corresponding to “always,” Alschuler says, reflecting “the extent to which the person is having thoughts that exemplify being willing to coexist with their pain versus the extent to which they are viewing their pain as a barrier that is difficult to overcome.” Overall, the ultrarunners were remarkably good at relying on adaptive coping (3.04 out of six, on average) rather than maladaptive coping (1.31 out of six). If that wasn’t the case, they probably would never have made it to one of these grueling races. Still, there were some interesting findings. For example, when runners used more than their usual level of maladaptive coping, they reported a greater perception that pain was interfering with their performance—even when the actual level of reported pain was held constant. They also spent more time thinking about their pain, which should be a reminder that sometimes it’s best not to dwell on it. The other interesting finding was a link between the use the maladaptive coping and the probability that a runner would finish the race. For every one-point increase in the maladaptive score, a runner’s likelihood of finishing the race dropped by a factor of three.Why head and face pain causes more suffering: Sensory neurons in the head and face tap directly into the brain's emotional pathways -- ScienceDaily
The team found that sensory neurons that serve the head and face are wired directly into one of the brain's principal emotional signaling hubs. Sensory neurons elsewhere in the body are also connected to this hub, but only indirectly. The results may pave the way toward more effective treatments for pain mediated by the craniofacial nerve, such as chronic headaches and neuropathic face pain. "Usually doctors focus on treating the sensation of pain, but this shows the we really need to treat the emotional aspects of pain as well," said Fan Wang, a professor of neurobiology and cell biology at Duke, and senior author of the study. The results appear online Nov. 13 in Nature Neuroscience.Even open-label placebos work, if they are explained -- ScienceDaily
For the first time, researchers from the University of Basel, along with colleagues from Harvard Medical School, have compared the effects of administering open-label and deceptive placebos. The team conducted an experimental study with 160 healthy volunteers who were exposed to increasing heat on their forearm via a heating plate. The participants were asked to manually stop the temperature rise as soon as they could no longer stand the heat. After that, they were given a cream to relieve the pain. Some of the participants were deceived during the experiment: they were told that they were given a pain relief cream with the active ingredient lidocaine, although it was actually a placebo. Other participants received a cream that was clearly labeled as a placebo; they were also given fifteen minutes of explanations about the placebo effect, its occurrence and its effect mechanisms. A third group received an open-label placebo without any further explanation. The subjects of the first two groups reported a significant decrease in pain intensity and unpleasantness after the experiment. "The previous assumption that placebos only work when they are administered by deception needs to be reconsidered," says Dr. Cosima Locher, a member of the University of Basel's Faculty of Psychology and first author of the study.Why Do Rich People Love Endurance Sports? | Outside Online
“By flooding the consciousness with gnawing unpleasantness, pain provides a temporary relief from the burdens of self-awareness,” write the researchers. “When leaving marks and wounds, pain helps consumers create the story of a fulfilled life. In a context of decreased physicality, [obstacle course races] play a major role in selling pain to the saturated selves of knowledge workers, who use pain as a way to simultaneously escape reflexivity and craft their life narrative.”Bring On the Exercise, Hold the Painkillers - The New York Times
It found that by reducing the production of prostaglandins, NSAIDs change how a body responds to exertion, this time deep within the muscles. For that study, researchers in the department of microbiology at Stanford University looked first at muscle cells and tissue from mice that had experienced slight muscular injuries, comparable to those we might develop during strenuous exercise. The tissue soon filled with a particular type of prostaglandin that turned out to have an important role: It stimulated stem cells within the muscles to start multiplying, creating new muscle cells that then repaired the tissue damage. Afterward, tests showed that the healed muscle tissue was stronger than it had been before.Power of shared pain triggers extreme self-sacrifice -- ScienceDaily
There were five hypotheses: shared experience promotes willingness to perform extreme pro-group action; shared negative experiences make individuals contribute more than euphoric experiences; the more intense the experience the stronger the pro-social effects; the effect of shared negative experiences on pro-social behavior is much stronger where groups compete directly against other groups rather than if they cooperate against nature; and the effects of shared negative experience can be stronger than those of kinship. The hypotheses were then tested empirically in a variety of different study populations, including U.S. military veterans of the Vietnam war, college fraternity and sorority members who had undergone hazing, English Premier League football fans, martial arts practitioners of Brazilian Jiu Jitsu who sometimes use painful belt-whipping, and twins to examine the level of fusion. From both the theoretical and empirical research, the study concluded that overall shared negative experiences are a powerful mechanism for promoting pro-social behaviors, which under certain conditions can be extremely costly to the individuals concerned.Opioids produce analgesia via immune cells: Researchers from the Charité find new signaling pathway -- ScienceDaily
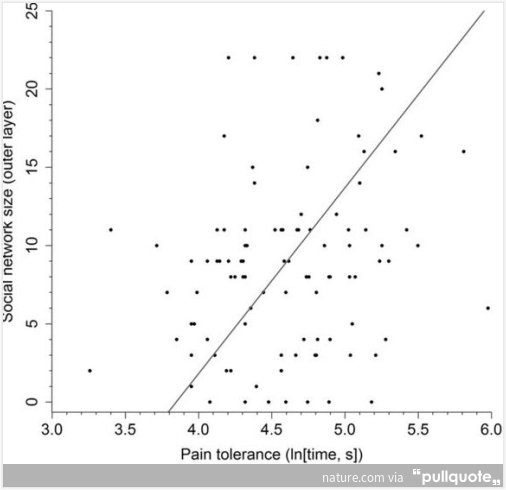
"We were able to show that opioid agonists activate opioid receptors on immune cells, which triggered the release of endogenous painkillers (opioid peptides) and produced analgesia in a mouse model of neuropathic pain," explains Prof. Machelska. She adds, "This led us to conclude that opioids can exert enhanced analgesia when they act directly in painful tissue -- providing that this tissue is inflamed and contain immune cells."Pain tolerance predicts human social network size : Scientific Reports